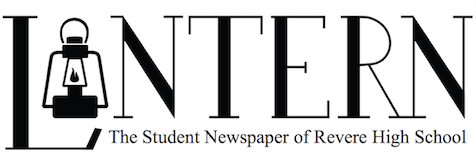
Recent pandemic compared to those in past
Compare and contrast of 2020 pandemic to the Spanish Influenza.
As seven year-old Jeanne Shinnick stepped onto her front-porch, she noticed something unusual about her quiet Florida neighborhood. Scattered throughout the front yards and even lining the street were bodies. Bodies of people and even their pets, with exciting long lives to live, gone forever. The culprit was a silent, invisible perpetrator: the Spanish Influenza.
After the Spanish Influenza took the life of Dr. Otto Werneke, his newly born daughter was baptized and placed next to his casket in an attempt to reduce gatherings by combining the funeral and baptism. Being forced to combine the sorrow passing onto heaven with the happiest welcome to God’s kingdom became a normal occurrence for those living in 1918.
As the pandemic of our generation, COVID-19, continues to rampage through daily life, people are reflecting back on the impact of the pandemic that also took so many lives nearly one-hundred years ago, the Spanish Influenza.
The Spanish Influenza pandemic, or the Spanish Flu, first showed up the United States in 1918. According to the CDC, there is still no universal consensus on where the virus originated, but researchers have identified that the virus was first noticed in the US on military personnel in spring of 1918. Quickly spreading from one person to another, around 50 million people died worldwide and nearly 700,000 people in the United States alone between 1918-1819. Nearly 500 million people, which was around one-third of the world’s population at that time, contracted the virus, and death rates were high for young children, middle aged adults and elderly people alike.
With little medical equipment and resources, the doctors of that time period could not produce a cure such as a vaccine or antibiotic to combat the H1N1 virus, as antibiotics were not discovered until nine years later. Doctors could not offer much more than supportive care. This led to many simple precautionary steps that people took to prevent spread, similar to the precautions people are taking right now as the vaccine awaits production.
Douglas Jordan of the CDC discussed the steps taken to limit the spread of the virus on the CDC’s website.
“With no vaccine to protect against influenza infection and no antibiotics to treat secondary bacterial infections that can be associated with influenza infections, control efforts worldwide were limited to non-pharmaceutical interventions such as isolation, quarantine, good personal hygiene, use of disinfectants and limitations of public gatherings, which were applied unevenly,” Jordan said.
In addition to a limit on equipment, no diagnostic tests existed for the virus. Furthermore, many doctors did not even know the cause of the illness, falsely attributing it to a bacterium called “Pheiffer’s bacillus (also known as Haemophilus influenzae).”
As both word and disease spread quickly, many people looked to the government to establish safety measures regarding the pandemic. This resulted in rules similar to those in place currently. Although Wildrow Wilson, president in 1918, failed to establish strict rules to counteract the virus, many cities established their own guidelines.
“Some cities managed to implement community mitigation measures, such as closing schools, banning public gatherings, and issuing isolation or quarantine orders, but the federal government had no centralized role in helping to plan or initiate these interventions,” Jordan said.
Since the original and arguably most notable flu outbreak of 1918, four pandemics have arisen in addition to many close calls, none of which have reached the magnitude of the most recent, COVID-19. Following the Spanish Flu, the next outbreak was caused by the then new influenza A (also known as H2N2 or the “Asian Flu”). After the virus emerged in East Asia in spring of 1957, it was discovered in the U.S. in coastal cities during the summer of 1957, where many people reported symptoms similar to today’s flu. According to the CDC, this pandemic accounted for 1.1 million deaths worldwide, and nearly 125,000 U.S. deaths.
The next outbreak was in 1968 with a different strain of influenza A (H3N2). This strain of the flu disproportionately affected elderly people and claimed the lives of over one million people worldwide and around 100,000 in the United States. People first noted the virus in the United States in September 1968.
The final pandemic before the Coronavirus outbreak was the flu outbreak of 2009. Although the death rates were not as high as in previous years, the virus infected many people and had unprecedented death rates in younger people. The CDC explained the effects of the 2009 flu pandemic on their website.
“The 2009 flu pandemic primarily affected children and young and middle-aged adults. The impact of the virus on the global population during the first year was less severe than that of previous pandemics,” the CDC said.
Even with these pandemics, it remains shocking to some scientists that it took the world this long for a deadly virus to spread. Throughout the last few years, the increased travel between countries and increased wildlife population have all been attributed to what researchers are calling the “perfect conditions for a wildfire.”
University of Liverpool Professor Matthew Baylis talked to BBC news about the history of potentially deadly pandemics leading up to the COVID outbreak.
“In the last 20 years, we’ve had six significant threats — SARS, MERS, Ebola, Avian influenza and Swine flu. We dodged five bullets but the sixth got us,” Baylis said.
Although it is likely that we will see another pandemic arise within the next one-hundred years, it is important to note that many significant medical improvements have occurred since the initial pandemic of 1918. Even with these improvements, there are still many things that occur globally that need to be solved before ruling out the idea of another pandemic.
“When considering the potential for a modern era high severity pandemic, it is important; however, to reflect on the considerable medical, scientific and societal advancements that have occurred since 1918,” Jordan said.